JMT Special Article: The Value of Medical Toxicologists
Source: Journal of Medical Toxicology (JMT)
Publication Date: June 19, 2025
Authors: Paul M. Wax, Tracy M. Kolian, Anthony F. Pizon
Keywords/Topics: Medical Toxicology, Poison, Poison Centers, Toxicology
JMT Special Article: The Value of Medical Toxicologists
Abstract
Poisoning is a major public health issue and one of the leading causes of injury related death in the US. Poisonings result from intentional or unintentional use of prescription drugs or illicit overdose including opioids, inhalation of toxic fumes, ingestion of contaminated food or drinking water, and envenomations. The cost of poisonings to US health care is large, especially when considering the costs of addiction and illicit opioids. As specially trained physicians, medical toxicologists play a major role in the treatment and care of poisoned patients while improving patient care, population health, and health care systems related to chemical exposures and poisonings including prevention. They also play a major role in the opioid epidemic and in caring for patients with opioid use disorder and substance use disorders more broadly. Regardless of these important roles, the recognition and knowledge of the value that medical toxicologists provide to health and the health care system is limited. As reimbursement becomes linked to outcome in a value-based care (VBC) market, medical toxicologists must continue to demonstrate their value to stakeholders. The American College of Medical Toxicology (ACMT) has long recognized the need for medical toxicologists to articulate their value and to advocate for themselves, the profession, and for the patients they serve. To that end, modeling infectious disease (ID) efforts in establishing value for their specialty, this paper outlines the ‘value’ of medical toxicologists in improving patient outcomes, and their positive impact on population health and health care systems.
Introduction
Poisoning is a major public health issue [1] and one of the leading causes of suicide and self-harm [1]. Poisonings result from intentional or unintentional use of prescription drugs or illicit overdose including opioids, inhalation of toxic fumes, ingestion of contaminated food or drinking water, and envenomations. Opioid overdoses are the leading cause of drug poisoning deaths in the US and are largely due to a rapid increase in synthetic opioids such as fentanyl [2, 3]. Altogether, the health care costs of poisonings are staggering [4, 5].
Medical toxicology is a subspecialty of medicine with a focus on the prevention, evaluation, treatment, and monitoring of injury and illness from exposure to drugs and chemicals, as well as biological and radiological agents. Important areas of medical toxicology include acute drug poisoning, adverse drug events, substance use disorders including addiction and withdrawal, environmental and workplace exposure to chemicals and radiologic materials, terrorism and emergency preparedness, and venomous bites and stings.
As specially trained physicians, medical toxicologists play a major role in the treatment and care of poisoned patients while improving population health and health care systems related to chemical exposures and poisonings including prevention. They also play a significant role in the opioid epidemic while caring for patients with opioid use disorder and substance use disorders more broadly [6,7,8].
Medical toxicologists often work within hospital systems, typically providing bedside consultations in the emergency department, intensive care units, and inpatient medical services where they provide real-time recommendations to other medical providers. They also provide medical direction to poison centers. They care for patients of all ages and different exposures including opioids and other substances of abuse. Unfortunately, many healthcare systems do not have access to medical toxicologists; in these instances, non-medical toxicologists, who often lack specific training in poisonings, treat these patients.
As a medical subspecialty, medical toxicology is not well known. A relatively new subspeciality, medical toxicology was first recognized by the American Board of Medical Specialties in 1992. Becoming a medical toxicologist requires a medical degree, a residency in a primary board specialty such as emergency medicine, two years of a medical toxicology fellowship, and passing a certification exam. 90% of medical toxicologists have completed residency in emergency medicine; others have completed residencies in pediatrics, internal medicine, preventive medicine, and psychiatry [9]. Very few medical toxicologists practice medical toxicology exclusively, due to challenges with compensation, patient volume, and difficulties in developing a robust full-time practice model. As with other medical subspecialties, the standard compensation model is a fee-based service, which is driven largely by volume and quantity of service. As a cognitive specialty that saves money by avoiding unnecessary testing, this model for determining compensation often undervalues medical toxicology care. In part, because of the variation in medical toxicologist roles, data regarding the positive impacts and the economic ‘value’ of medical toxicologists on patient care directly as well as the health care system is limited.
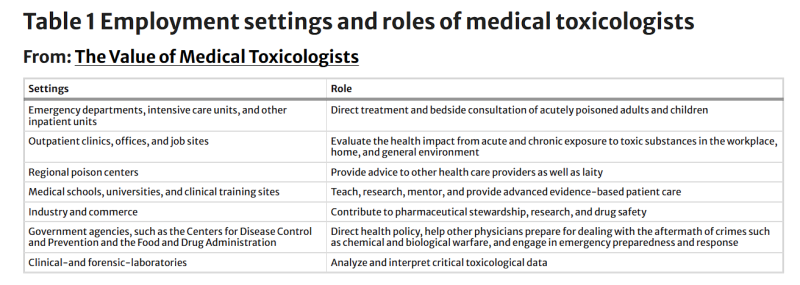
In short, medical toxicologists work in a myriad of settings and roles (as summarized in Table 1). Ironically, it is largely because of these myriad roles that the value of medical toxicologists in improving patient outcomes and the efficiency of health care systems is difficult to quantify.Table 1 Employment settings and roles of medical toxicologists.
The American College of Medical Toxicology (ACMT) recognizes and strives to convey the value of medical toxicologists to various stakeholders. Modeling the efforts of infectious diseases (ID) in establishing their value [10, 11], this paper outlines the ‘value’ of medical toxicologists in improving patient outcomes, and their positive impact on population health and health care systems (as summarized in Table 2).
Medical Toxicologists Improve Outcomes
The triple aim of health care (improving population health, enhancing the care experience, and reducing costs) is the guiding principle for health care improvement and has been the focus of the US national strategy for health care since 2010 [12]. A 2022 editorial in Frontiers of Public Health defined value as the following: “Value is not about quality or technical outcomes alone, any more than value is about prices and costs alone—although both are constraining factors” [13]. Today ‘value’ means the simultaneous pursuit of improving patient outcomes, improving patient experiences, lowering long-term costs by reducing or eliminating waste, and taking responsibility for the wellness of the caregiver workforce” [13]. Hence, in part, value is created by improving the outcomes of patients with a particular clinical condition, while simultaneously taking into account the cost of achieving that improvement [14, 15].
Measuring value for individual providers and specialties is becoming increasingly important. Value-based care (VBC) is a model linking reimbursement to improved patient quality, safety, and outcomes [16]. This model is an enticing idea to improve patient outcomes while reducing healthcare costs. Yet, to have any relevance, specialties must demonstrate their value to stakeholders. The VBC model is a paradigm shift in health care delivery. Therefore, to have any relevance in this new model, specialties must have a means to demonstrate improved outcomes if VBC is widely adopted. Without demonstrable value, a specialty may not sustain itself.
To assess value, health care providers must measure patient outcomes using relevant metrics such as reduced mortality, reduced hospital length of stay, reduced adverse events, and improved patient experience. Innately, medical toxicologists apply the triple aim approach in their daily work through multiple ways. Medical toxicologists believe that they improve patient outcomes and mortality, lower costs, advance health equity, and improve population health based on their response to community level exposures such as emergency chemical spills and toxic exposures in consumer products. But what is the evidence?